
Trisoma®
Myofascial Trigger Point Therapy
 Muscle pain is one of the more frequent causes of dysfunction of modern man, yet it is frequently easy to treat without medications.[38]
One of our clients described the the modality as:
"clothes on, no oil, pain gone™"
Muscle pain is one of the more frequent causes of dysfunction of modern man, yet it is frequently easy to treat without medications.[38]
One of our clients described the the modality as:
"clothes on, no oil, pain gone™"
Common Cause of Pain, but Most Practitioners Treat Only Symptoms
Active trigger points are hyperirritable small groups of cells in skeletal muscle and surrounding connective tissue that can produce local or referred pain and other symptoms. Many ailments, such as mock sciatica, carpal tunnel syndrome, migraine headaches, brachial plexus issues, can be significantly managed or totally eliminated with trigger point therapy. Have you ever had a headache, clonus or twitching muscles, after a massage? The massage might have felt great, but most probably your therapist activated trigger points on your body. Only a medical professional can provide a diagnosis, but a qualified massage therapist may provide relief of myofascial pain after simple assessments. If relief is not found in 1-3 treatments, then you may be referred to other modalities, such as medical, chiropractic, osteopathic or physical therapy.
Muscle tissue is the largest organ in the body; it is metabolically active, filled with nerves and the “primary target of the wear and tear of daily activities, but it is the bones, joints, bursae and nerves on which physicians usually concentrate their attention.”[1c]
The Journal of Bone and Joint Surgery, and the Journal of the American Osteopathic Association, have both published papers recently showing that physicians simply do not have an adequate understanding of musculoskeletal medicine health care.
Many people have some muscles that are not pain free, and in most cases, muscle ailments involve active Trigger Points.
https://www.sigmaaldrich.com/US/en/tech-docs/paper/77496?msclkid=7cd00b70bdcd1002d3766d722ff9d4a8&utm_source=bing&utm_medium=cpc&utm_campaign=applied_dsa_pdp_NA_(bing%20ebizpfs)&utm_term=sigmaaldrich&utm_content=Applied_PDP
https://www.kenhub.com/en/library/anatomy/the-neuromuscular-junction-structure-and-function
https://www.ncbi.nlm.nih.gov/books/NBK470413/
https://biologydictionary.net/neuromuscular-junction-2/
https://www.jove.com/science-education/14840/the-neuromuscular-junction

Do you have trigger points?
Check the boxes:Muscles are sensitive to pressure
Stiff, tight, spasmic feeling
Headache
Dull, aching, or burning pain in muscles
Pain going down the arm or leg
Numbness
Muscle imbalances
Unpredictable, erratic symptoms
Heat eases the pain
If you checked many of these, then you probably have active trigger points.
Etiology of Trigger Points
Travell and Simons defined TrP's as discrete, focal, hyperirritable spots located in a taut band of skeletal muscle[30], which are painful on compression and can produce local and referred pain which can perplex medical professionals not familiar with trigger points. A current theory for the cause of a trigger point is that the calcium switch fails to turn off in the sarcomere. Symptoms can include: tenderness, burning, numbness, weakness, reduced range of motion, motor dysfunction, and various autonomic phenomena, including temperature, sweating, dryness, dizziness, vision problems and others [1a]. Such trigger point maladies are common in athletes, dancers, musicians, as well as in the typical slumped-over office worker. Repetitive strain injuries (RSIs)[4] are sometimes actually referred from trigger points. If trigger points are left untreated, they may cause irreparable damage to muscle fibers, and long-term changes to the nervous system. Trigger Points have been photomicrographed[32], measured electrically[32], imaged by modified MRI[33], and even tissue biopsy sampled for toxicity[34], so if your health professional does not diagnose nor treat them, then ask why not?Most trigger points can be reduced or extirpated by:
- needling,
- medical acupuncture,
- electric stimulation [7],
- Trigger Point injections (CO2 or prolocaine)
- prolotherapy (dextrose injections, etc.)
- manual Trigger Point therapy (ischemic compression massage)

Manual therapy can't be administered with a lucrative tablet,
is difficult to patent, and can't be sent through the mail. Massage therapists do not have powerful political lobbyists, nor the advertising money of pharmaceutical corporations so you may not see trigger point therapy on TV or in medical school.[8] “Structuralism” is an excessive clinical focus on posture, alignment, and symmetry and other biomechanical factors — crookedness, in other words, or what I call the “biomechanical bogeyman.”[35] Therapists who are into structuralism attribute virtually all pain problems to alleged biomechanical deficiencies that are either entirely imaginary (sometimes absurd), or just relatively unimportant factors in most cases. [36] As Trisoma states, "a good chiropractor is great if you have a chiropractic problem."Trisoma does not use drugs nor injections,
but the simplest and least invasive methods of direct pincer palpation (locating manually and pressing or holding firmly using thumb and finger), elbows and feet, as in Barefoot Deep Tissue Therapy. After release of trigger points in a muscle, several seconds of gentle stretching can help "reset" the muscle, however stretching of affected muscles is recommended only if there is no pain, since muscle strands containing trigger points may be strained before the surrounding fibers "feel" a stretch. If 1-3 therapy visits do not produce relief, then referral is recommended. Paul also can teach clients how to work manually on themselves for many cases. Paul studied under John Harris, an Olympic Massage Therapist who has written books, videos and taught Trigger Point Therapy at the Santa Barbara Body Therapy Institute.Trigger points activate from several causes, such as acute or chronic muscular overload due to trauma, overuse, poor posture, chilling of a muscle and even emotional stress. This could be from repeat movement, or from low force, long-term static holds of posture, or even holding a pencil for too long. Once a trigger point has activated, due to metabolic stasis in the area of the TrP, waste products begin to accumulate. These waste products are nerve irritants (bradykinin, serotonin, hyaluronic acid, etc.) which, in turn, produce and perpetuate pain signals. Due to the accumulation of waste products, the blood supply to the area is decreased, resulting in a contracture (tight band) of muscle fibers and ischemia and resultant pain are felt by the patient.[5] Left untreated, constant pain signals can make the brain decide to turn off the muscle, and leave some fibers contracted, as in frozen shoulder.

Pain Sources May Be Elusive
Active trigger points frequently refer pain to other areas of the body, sometimes causing an imbroglio of misdiagnoses, including sciatica and carpal tunnel syndrome and gynecological opinions, and failure of convention medical treatments (surgery and drugs) to relieve symptoms. However the referral patterns have been well-defined and catalogued over the years. An example is a trigger point in the piriformis or gluteal muscles causing sciatic-like pain, which some doctors may misdiagnose as spine trouble; or arm and neck trigger points which mimic carpal tunnel syndrome. Why does the pain occur away from the trigger point? There are different theories: one in very simple terms is analogous to peripheral neuropathy, where nerves for the toe are wired to the "toe" area of your brain, and no matter where the 3 foot long "toe" nerve is affected along its length, pain is felt in the toe. Other examples of referred pain are arm pain for heart attacks, "brain freeze" after drinking a cold liquid, scratching your ear to relieve the tickle in your throat and "phantom pain" in an amputated limb caused by mapping in the brain. Myofascial pain should not be confused with Myofascial Release.Chronic pain has been found to cause reorganization of the central nervous system which amplifies neural activity at multiple levels of the somatosensory system even before the appearance of clinical paresthesia symptoms, even with no change in peripheral pain signals.[29] This means that the spine, brainstem, and cortical structures of brain reorganize due to nerve signals before the affected area becomes painful, tingling, numb or spasmic. Additionally, the stimuli are also thought to "unmask silent connections between neural region mapping" of different body parts. Such physical changes may help explain trigger point phenomena. Patient complaints that originate in the musculoskeletal system usually have multiple causes responsible for the total picture,[1b] but Trigger Point Therapy is used for myofascial pain syndromes, which may include headache (tension and migraine), neck, jaw, shoulder, arm, back, leg and various other local or referred symptoms.
Despite the overwhelming evidence of its effectiveness in 60 years of medical journals,[2] trigger point therapy finds few allies in the mainstream medical community, who find it difficult to admit that a skilled massage therapist may possibly remove myofascial pain that a highly trained, and highly paid, physician has failed to remove. A variety of drugs discovered by serendipity from diverse pharmacological classes are in use for migraine prevention.[28] Current trends in migraine prophylaxis include inhibition of cortical hyperexcitability, nociceptive dysmodulation and surgical closure of patent foramen ovale. However migraines are often accompanied by trigger points in the suboccipital and/ or rhomboid muscles, and when deactivated, the pain may be reduced or eliminated.
Research on theories about trigger points is continuing, but in 2008 trigger points have been documented by MRI. (Click for more info.) Previous theories include muscle scarring, contractured sarcomeres and abnormality at the neuromuscular junction.
New Research:
- "Nociceptive inputs in active TrPs could lead to muscle atrophy of the involved muscles." (Association of Cross-Sectional Area of the Rectus Capitis Posterior Minor Muscle with Active Trigger Points in Chronic Tension-Type Headache: A Pilot Study. American Journal of Physical Medicine & Rehabilitation. 87(3):197-203, March 2008.)
- The National Institutes of Health Clinical Center is sponsoring new research to investigate the biochemistry of trigger points in the trapezius, a large muscle lying between the neck and shoulder. According to the NIH, trigger points in the muscle are typically caused by emotional stress, postures such as hunching shoulders, certain activities like using a telephone receiver without elbow support, or by wearing certain articles such as a heavy coat or heavy purse. (Protocol Number: 02-CC-0245)
- The American Headache Society published that injecting Botox may cut the number of migraines by preventing activation of a muscle which plays a role in migraines.[3] What this means is that a trigger point is relieved by paralyzing the muscle with a drug.
- Acupuncture meridians have not yet been verified by Western medicine, but in January 2007, research was published by the American Journal of Physical Medicine & Rehabilitation showing that acupuncture points were found to have a significantly decreased number and density of subcutaneous myelinated peripheral nerve structures.[6]
- The Journal of the American Medical Association reported that frequent migraine sufferers felt better after acupuncture (which sometimes may relax trigger points.) Trigger points are not the same as acupuncture points, but research is being begun by mainstream organizations on the anatomic morphology and histology of acupuncture and trigger points.
- Trigger Point Injections: Simple Explanation
- Trigger Points Conspectus: Explanation, Diagnosis and Management
- Myofascial Pain Syndromes
- Trigger Points for Trainers and Clients
- Fibromyalgia
- Headaches
- Headache Case Study
- Needling and Acupuncture for Headaches
- Tension Myositis Syndrome
- More Trigger Point History
"Life is like a bicycle. You don't fall off until you stop pedaling." - Dr. Travell
Long History; Recent Revival
Trigger point therapy was practiced for hundreds or thousands of years in Asia and probably Europe, and continues in China within Tui Na practice, and in Europe in musculoskeletal medicine. Before pharma rolled over Western Medicine, the British were publishing articles investigating referred myofascial pain. In the 1940's Dr. Janet G. Travell researched myofascial pain when physical medicine was still common, using prolocaine and her father's electric discharge machine, and by treating these points, the pain would not only cease, but the cessation of the pain reflex would restore muscle function. Dr. Travell began cataloguing trigger points for predictable referred pain patterns as her patients improved.
When Senator John F. Kennedy first consulted Dr. Travell in the spring of 1955, for muscle spasms in his left lower back that radiated to his left leg and made walking prohibitive, he was questioning his ability to continue his political career. Dr. Travell's “trigger point” therapy proved effective,[10] and the Senator later became President, with Dr. Janet G. Travell as President Kennedy's physician.
Dr. David G. Simons joined Dr. Travell to publish medical books, and later finally validated MTrPs by MRI. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8448923/ and various treatment techniques have been accepted by medical insurance, such as Blue Shield, despite most physicians not being trained in such methods. Unfortunately most medical doctors, and even many chiropractors, massage and other therapists, are not trained or skilled, or do not seem to desire to spend 20 minutes assessing and manually working on a patient. Many acupuncturists, if trained in Tui Na, will notice that TrPs are near some acupuncture points, which seem to be evidently points along the myofascial planes.
Since then Trigger Point Therapy has been used successfully by doctors and massage therapists on many clients who have suffered under the depredation of chronic myofascial pain with no relief from surgery or drugs. [More TrP History]https://journals.lww.com/ajpmr/abstract/2021/10000/assessment_of_myofascial_trigger_points_via.12.aspx Biomechanical properties and blood flow of active and latent myofascial trigger points assessed via imaging were found to be quantifiably distinct from those of healthy tissue.
References
2. Davies, Clair. (2001). The Trigger Point Therapy Workbook: Your Self-Treatment Guide for Pain Relief
(There has been an explosion of Trigger Point Therapy books in recent years! This one is an economical vade mecum.) (Return to Reference 2 in text)
3. 47th Annual Scientific Meeting. (2005). American Headache Society (Return to Reference 3 in text)
4. Office Place RSIs Decreased in 1994, InteriorsAndSources.com, September 1996. (Return to Reference 4 in text)
5. Sheila Laws, D.C., NIMMO-Receptor Tonus Technique, The American Chiropractor, Volume 24, Issue 02 Published 10/30/2005 (Return to Reference 5 in text)
6. Wick, Franziska MD; Wick, Nikolaus MD; Wick, Marius C. MD Morphological Analysis of Human Acupuncture Points Through Immunohistochemistry. Research Article, American Journal of Physical Medicine & Rehabilitation. 86(1):7-11, January 2007. (Return to Reference 6 in text)
7. The Immediate Effectiveness of Electrical Nerve Stimulation and Electrical Muscle Stimulation on Myofascial Trigger Points, American Journal of Physical Medicine & Rehabilitation. 76(6):471-476, November/December 1997. Hsueh, Tse-Chieh MD, MS 2; Cheng, Pao-Tsai MD, MS; Kuan, Ta-Shen MD, MS; Hong, Chang-Zern MD (Return to Reference 7 in text)
8. National Institutes of Health (NIH), http://www.nih.gov/ (Return to Reference 8 in text)
10. James E. Bagg, Jr.; The President's Physician, Texas Heart Institute Journal. 2003; 30(1): 1–2. (Note: Paul Svacina volunteered at the Texas Heart® Institute and Emergency Department at St. Luke's Episcopal Hospital in the Texas Medical Center, Houston, in the 1980's) (Return to Reference 10 in text)
28. Nabih M. Ramadan, MD. (2007) Current Trends in Migraine Prophylaxis Headache: The Journal of Head and Face Pain 47 (s1) , S52–S57 doi:10.1111/j.1526-4610.2007.00677.x Department of Neurology, Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL, USA. (Return to Reference 28 in text)
29. Michele Tinazzi1, Antonio Fiaschi1, Tiziana Rosso1, Franco Faccioli2, Johannes Grosslercher2, and Salvatore M. Aglioti3. Neuroplastic Changes Related to Pain Occur at Multiple Levels of the Human Somatosensory System: A Somatosensory-Evoked Potentials Study in Patients with Cervical Radicular Pain. The Journal of Neuroscience, December 15, 2000, 20(24):9277-9283. Dipartimenti di Scienze Neurologiche e della Visione, 1: Sezione di Neurologia Riabilitativa and 2: Sezione di Neurochirurgia, Università di Verona, 37134 Verona, Italy, and 3: Dipartimento di Psicologia, Università di Roma "La Sapienza," and Istituto di Ricovero e Cura a Carattere Scientifico, Fondazione Santa Lucia, 00179 Rome, Italy (Return to Reference 29 in text)
30. David J. Alvarez, D.O., and Pamela G. Rockwell, D.O., Trigger Points: Diagnosis and Management. Feb. 15, 2002. American Family Physician Journal, of the American Academy of Family Physicians. David J. Alvarez, D.O., East Ann Arbor Health Center, 4260 Plymouth Rd., Ann Arbor, MI 48109. University of Michigan Medical School, Ann Arbor, Michigan (Return to Reference 30 in text)
32. David G Simons, Siegfried Mense and IJ Russell, Muscle Pain: Understanding Its Nature, Diagnosis and Treatment Chapter: Myofascial Pain Caused by Trigger Points p. 205–288 (1st hardcover edition), 2000, Lippincott Williams & Wilkins (Return to Reference 32 in text)
33. Chen et al., p. 2 2007, Archives of Physical Medicine and Rehabilitation (Return to Reference 33 in text)
34. Jay P. Shah MDa, Corresponding Author Contact Information, E-mail The Corresponding Author, Jerome V. Danoff PhD, PTa, b, Mehul J. Desai MDc, Sagar Parikh BAa, Lynn Y. Nakamura MDd, Terry M. Phillips PhD, DSce and Lynn H. Gerber MDf, Biochemicals Associated With Pain and Inflammation are Elevated in Sites Near to and Remote From Active Myofascial Trigger Points Copyright © 2008 American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation Published by Elsevier Inc. (Return to Reference 34 in text)
35. Paul Ingraham, Registered Massage Therapist (Vancouver), Your Back Is Not “Out” and Your Leg Length is Fine - The story of the obsession with crookedness in the physical therapies p. 2 2009 Feb. 1, http://saveyourself.ca/articles/structuralism.php (Return to Reference 33 in text)
36. Paul Ingraham, Registered Massage Therapist (Vancouver), Save Yourself from Trigger Points and Myofascial Pain Syndrome! 2009 Feb. 1, http://saveyourself.ca/tutorials/trigger-points.php (Return to Reference 36 in text)
37. Susan Parker, PT, OBGYN.net Editorial Advisor, The Iliopsoas Trigger Point Retrieved 2009 Feb. 15, http://www.obgyn.net/pelvic-pain/pelvic-pain.asp?page=articles/parker_Iliopsoas_Trigger_Point (Return to Reference 37 in text)
38. Claim by Paul Svacina, P.E. (Return to Reference 38 in text)
Images
1.
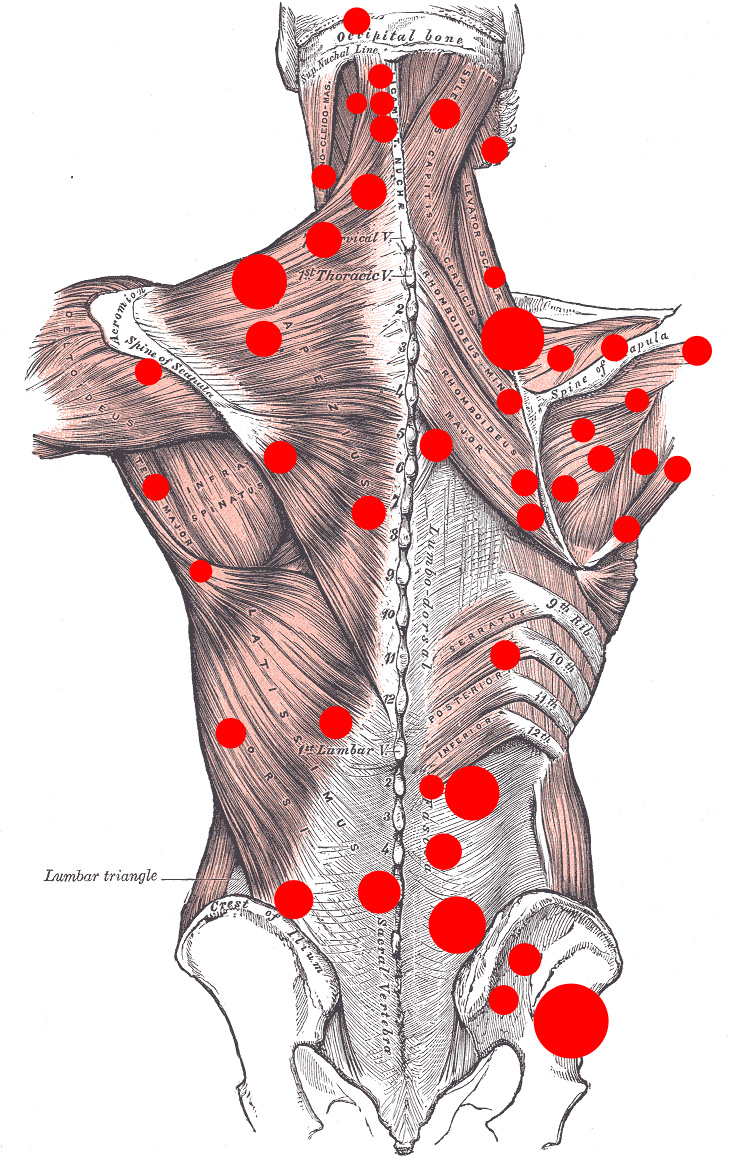
Paul Svacina 2008. Modified image of Muscles connecting the upper extremity to the vertebral column, by
Gray, Henry.
Anatomy of the Human Body. Philadelphia: Lea & Febiger, 1918; Bartleby.com, 2000. www.bartleby.com/.
(Return to Image 1 in text)
2.
Paul Svacina,
Ellwood, 2008.
(Return to Image 2 in text)
3.
& 4.
Courtesy of freeimages.co.uk
(Return to Image 3 in text)
(Return to Image 4 in text)